Examining Claims of mRNA Vaccines and Multiple Sclerosis
Written on
Chapter 1: Understanding the Claims
The assertion that mRNA vaccines are linked to multiple sclerosis has recently gained traction on social media, particularly Twitter, where a paper from the World Health Organization (WHO) has been cited as evidence. This paper, however, is not what it seems.
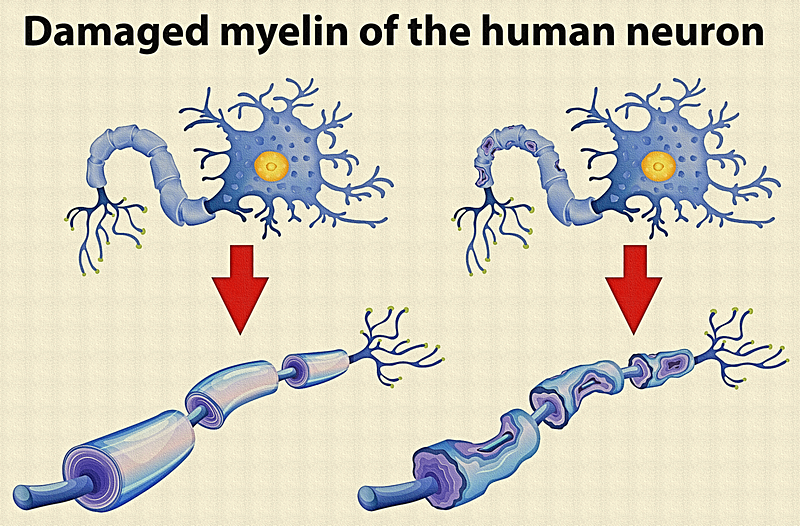
Multiple sclerosis (MS) is recognized as the most prevalent neurological disorder causing disability among younger populations. This condition arises when the immune system erroneously targets the myelin sheath, which surrounds nerve fibers and is crucial for efficient electrical signal transmission. Although not directly fatal, MS is a chronic ailment that leads to a range of debilitating symptoms, including fatigue, vision impairment, muscle spasms, and cognitive difficulties. Living with MS is not ideal.
So, does this claim hold any scientific merit? Yes, while the research cited is scientifically valid, it consists of just two individual cases. Let’s delve into the findings presented in this paper and evaluate the implications for the safety of mRNA vaccines.
Section 1.1: Overview of the Study
This particular study has yet to undergo formal publication; it was shared as a poster at a conference organized by the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS) in 2022. Such presentations often serve as preliminary reports of scientific findings that may later appear in full publications.
Contrary to popular belief, this paper has not been published or endorsed by the WHO; it simply appears in the WHO COVID-19 Research Database. The study by Qiu et al. from the University Hospital of Zürich, Switzerland, documented two instances of MS emerging shortly after mRNA vaccination. The research was led by Roland Marin, a well-respected neurologist and expert in MS.
A noteworthy aspect of the study is its investigation into spike protein-activated T-cells derived from the blood and cerebrospinal fluid of the two patients. They discovered that these activated T-cells reacted not only to spike protein but also to proteins associated with the myelin sheath, including:
- Myelin basic protein (MBP)
- Myelin oligodendrocyte glycoprotein (MOG)
- Proteolipid protein (PLP)
To affirm that these T-cells were indeed activated by the spike protein, the researchers demonstrated their ability to bind both spike proteins and myelin sheath proteins in a controlled lab setting, where pro-inflammatory molecules were also identified, indicating activation.
The phenomenon known as molecular mimicry likely accounts for the cross-reactivity between spike and myelin sheath proteins. This is not unexpected; molecular mimicry is an established factor in the pathogenesis of MS, occurring when foreign peptides share similarities with those of the host’s cells, potentially leading immune responses to target both.
Subsection 1.1.1: Limitations of the Study
Despite the intriguing findings, the case study by Qiu et al. comes with limitations. While it establishes a biological basis for the possibility that spike proteins may trigger MS via cross-reactive T-cells, it does not definitively link the spike protein to the mRNA vaccine.
The timing of the vaccine and the onset of MS raises concerns, but without testing for SARS-CoV-2, it remains uncertain if the T-cells were activated by the vaccine's spike protein or that of the virus itself.
Section 1.2: Contextualizing the Evidence
Various case studies have emerged suggesting a connection between MS and COVID-19 vaccinations; however, the authors often caution that correlation does not imply causation. Qiu et al.’s case study is unique in presenting credible biological evidence for a potential link between mRNA vaccines and MS.
However, it’s crucial to note that case studies rank among the weakest forms of scientific evidence. They are challenging to replicate and do not represent the broader population. Without control groups, we cannot ascertain whether mRNA vaccination truly elevates the risk of MS compared to individuals who are unvaccinated.
In larger cohort studies that included control groups, no significant increase in demyelinating events has been observed following mRNA vaccination. For instance, a 2021 study involving over 30 million participants found no notable association between COVID-19 vaccines and demyelinating disorders. Conversely, SARS-CoV-2 infection was linked to a 1.7-fold higher risk of such events.
A 2022 analysis from the WHO’s VigiBase identified a total of 15,616 neurological adverse events following vaccination with the Pfizer mRNA vaccine, with only one case of MS reported, yielding a rate of 0.006%. This figure would decrease dramatically when considering the total number of vaccine doses administered.
Chapter 2: Misinterpretations in Public Discourse
The viral tweet that initially propagated the theory that mRNA vaccines are responsible for MS referenced my academic research, misrepresenting its content to support this assertion.
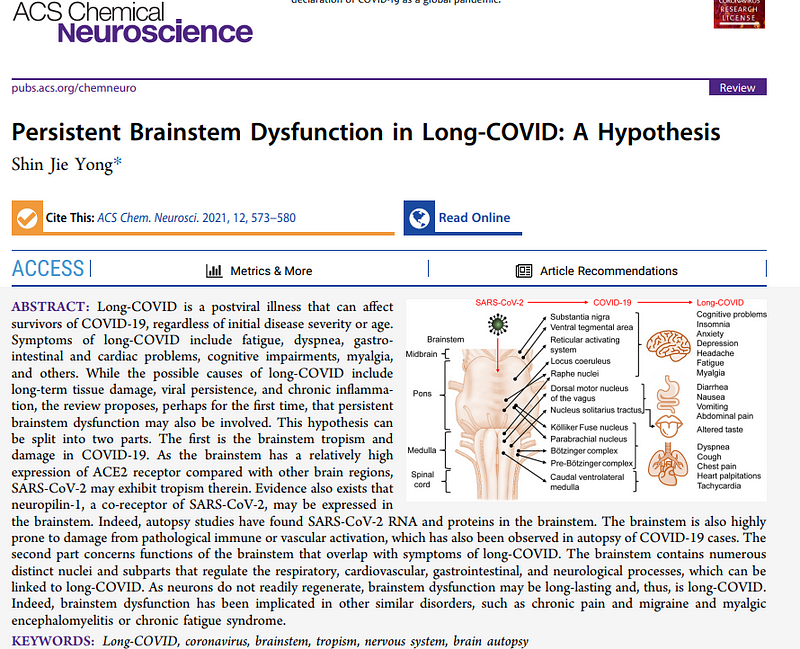
The image mentioned in this tweet was taken from my 2021 paper, “Persistent Brainstem Dysfunction in Long-COVID: A Hypothesis,” published in ACS Chemical Neuroscience. In that work, I explored potential mechanisms of long COVID, drawing on various studies related to brain function.
It’s perplexing to see how my research on brainstem functions could be linked to claims regarding mRNA vaccines and MS. The biological connections asserted are fundamentally flawed, and it is alarming how many individuals have accepted this misinterpretation.
If you've reached this point, thank you for engaging with this content. If you wish to stay updated, consider subscribing to my Medium email list. For those interested in additional access, using my referral link to become a member will also support my work. Your generosity is appreciated.